Children’s Vision
CHILDREN’S VISION
WHAT IS CHILDREN’S VISION & BEHAVIOURAL OPTOMETRY?
Children’s Vision and Behavioural Optometry is a philosophy of vision care that looks beyond the health and clarity of sight. It is an expanded area of optometry that looks at the functioning of the eyes and the brain together, rather than individually.
WHAT ARE BEHAVIOURAL OPTOMETRISTS?
Behavioural optometrists have a special expertise in children’s vision, patients with learning-related vision problems, traumatic brain injury, binocular vision dysfunction, as well as training in enhancing visual skills for different sports.
OUR CHILDREN’S VISION EXPERTS

NICK HANSEN
Childrens-visionis a Past President of The Australasian College of Behavioural Optometrists (ACBO) which is the prime educator for Australian, New Zealand and Asian optometrists in Behavioural optometry. Nick’s main expertise is with children with strabismus (eye turn) and amblyopia (lazy eye). In this area, he has published numerous papers and spoken at various Optometric and Educational Courses both nationally and internationally.
Book an appointment with one of our experts today.
AMBLYOPIA
WHAT IS AMBLYOPIA?
Amblyopia (or lazy eye) is where the eyesight in one eye is worse than in the other and that correcting the eyesight (with spectacles or contact lenses) does not improve the vision.
The three most common causes of Amblyopia are:
1. A large refractive error in one or both eyes.
2. Congenital cataracts.
3. An eye turn.
SYMPTOMS
Generally the patient experiences no symptoms apart from the possible awareness of poor eyesight in that eye when they cover up the good eye.
TREATMENT
1. Remove the cause of the amblyopia.
- Correct any refractive error with spectacles/contact lenses, remove any cataract or treat the eye turn.
- This may restore the eyesight without any further treatment required.
2. Start visual therapy.
- Most people with amblyopia need visual therapy as well as treating the underlying cause. This is because the drop in eyesight is not because the eye cannot see. Once any refractive error is compensated the amblyopic eye will be receiving a clear normal image.
- The eyesight however may still be poor because the brain is still ignoring or suppressing the image from the amblyopic eye just like it did prior to treatment.
- Visual therapy, including patching the good eye, is undertaken to stimulate the brain to pay attention to the amblyopic eye.
- In reality amblyopia is not so much about the ‘lazy eye’ but rather the brain (visual cortex) having learnt to turn off (suppress) the blurry picture from the amblyopic eye so that it does not interfere with the picture from the good eye.
DURATION OF TREATMENT
- Age should not be a deterrent at any attempt to improve visual acuity. Research has shown that the younger we treat amblyopia the more likely we are to restore normal eyesight.
- There is not critical period as such, but rather it becomes more and more difficult to improve visual acuity as the child gets older.
- In those cases where the amblyopia is due to an eye turn, the amblyopia has to be treated before the eye turn can be treated.
- It takes between 3-6 months of visual therapy to achieve the above goals in most cases of amblyopia.
- The visual therapy will need to be monitored, and the patient reassessed in office, every 2-4 weeks.
- In severe cases of amblyopia, normal eyesight may not be fully achieved or will take a longer length of time.
- Once cured the spectacle correction may still be required to ensure the amblyopia does not return.
- If patching is required it need to be done for a minimum of 2 hours per day.
- Patching is not done at school but rather at home while doing assigned visual therapy activities.
STRABISMUS
WHAT IS STRABISMUS?
Strabismus (eye turn) is a visual problem where the eyes are not aligned properly causing the eyes to point in different directions.
UNDERSTANDING THE CONDITION
The first thing to understand is that the eye turn does not worry your child. They are not in any pain or discomfort, they can see clearly (out of the straight eye) and as far as they are concerned they can’t see what all the fuss is about. This is because when one eye is not looking at the same thing that the other eye is looking at the brain learns to turn it off so as not to see two of everything. This is called suppression and if it occurs long enough then the eye that’s being turned off won’t develop normal eyesight, eye movement skills and eye processing (perception) abilities.
WHY DID MY CHILD DEVELOP AN EYE TURN?
Genetic Factors: About 7% of children between the ages of 6 and 17 years have an eye turn. Of these 47% have a family history of an eye turns.
TYPES OF EYE TURN
CONGENITAL
- Only a very small percentage of children are actually born with an eye turn.
- Some develop an eye turn very soon after birth (in the first 2 to 4 months).
- The actual underlying cause is not fully understood.
- Surgery is usually required for this type of eye turn in the first 12-24 mths of life.
ACQUIRED
1. Due to a Significant Refractive Error in one or both eyes.
- A large degree of long sightedness in one or both eyes can cause an inward eye turn.
- Whenever we drive our focusing system it stimulates the eyes to converge (turn in).
- Normally we can control this convergence and maintain normal eye alignment except when very tired or if we have a large amount of long sightedness to also overcome.
- Often this type of turn is first noticed when the child is becoming more involved in prolonged close work around the age of 2 to 4 years.
2. Due to a High Accommodative Convergence Ratio.
- Some individuals have an excessive stimulation to converge the eyes whenever the eyes try to focus up close.
- This is called a high Accommodative Convergence Ratio.
- Even with relatively low degrees of long sightedness or little near work demand the eyes get excessive stimulation to converge.
- Eventually the brain learns to leave one eye in and turn it off to alleviate the stress and demand of trying to keep the eyes turned out.
TRAINING THE EYE
Spectacles to train the eyes straight:
- Spectacles (or contact lenses) compensate for the long sightedness and reduce the stimulation to converge the eyes.
- In 80% of cases spectacle lenses combined with visual therapy will achieve a functional cure.
- Spectacles must be worn constantly to achieve this and may need to be in a bifocal or multifocal design to achieve the fastest results.
VISUAL TRAINING
- Visual training isn’t just about doing exercises on eye muscles.
- Visual training is also about teaching the brain how to straighten the eyes and developing the mechanism by which it can maintain the eyes straight.
- Depending on how long the eyes have been turned it can take 6 to 18 months before normal stable binocular vision is fully established.
SURGERY
- In most cases it is not a matter of operating on an eye muscle to pull the eye straight. This may well give a cosmetic improvement but fails to address the underlying cause of the turn and hence will fail to develop normal binocular vision. (i.e. Functional Cure.)
- Surgery is most successful in treating Congenital turns, turns due to muscle palsy and in cases where therapy has not produced a good cosmetic outcome.
- Surgery is generally not successful at achieving a functional cure for Acquired eye turns.
ACCOMMODATIVE DYSFUNCTION
WHAT IS ACCOMMODATIVE DYSFUNCTION?
Accommodative dysfunction is when a patient has a problem sustaining prolonged near focus. This is not an eyesight or refractive error problem but rather an acquired fatigue problem which produces eye strain and stress with prolonged near work.
WHAT IS CAUSING A FOCUSING PROBLEM?
There are four reasons for developing an accommodative dysfunction;
- Poor general health (chronic fatigue syndrome, glandular fever, bad flu etc.)
- A side effect of some medications. (Ritalin, antihistamines, etc.)
- A high degree of long-sightedness or eye turn (especially esotropia).
- Near point stress due to prolonged near tasks; particularly if at an age where you have not yet developed good focusing stamina to cope with it.
Note: accommodative dysfunction can even happen in the adult eye, especially if you are doing a stressful near centred task (eg new job involving more close work, study, prolonged computer work, fine sewing etc).
SYMPTOMS
The symptoms associated with focusing dysfunction are usually related to the task that produces the stress, that is, prolonged near centred tasks. The symptoms may include, but are not limited to the following:
- Visual stress symptoms include: red eyes, sore eyes, transient blurry vision and/or headaches.
- Difficulty sustaining near vision attention (may actually avoid near tasks).
- Glare symptoms while doing close work, this includes pages or computer screens.
- Abnormal posture adaptations such as head tilt or moving work closer.
TREATMENT
1. Training spectacle lenses for all close work.
- The problem is not that things are constantly blurry, the problem is that the focusing system is working too hard to keep it clear, this causes fatigue.
- The training lenses help alleviate the visual point stress.
- The more they are worn for near work, the sooner the patient will have better focusing stamina, this also means that the sooner the patient will no longer need to wear glasses.
2. Eye exercises (vision therapy).
Visual Therapy on its own is slow to develop accommodative (focusing) stamina for the simple reason that for every half hour of therapy that might be done at night time, the child/adult has usually been doing 5 or 6 hours of “anti-therapy” during the day (i.e. demanding close work causing accommodative fatigue).
DURATION OF TREATMENT
Generally the training lenses are needed to be worn for all close work including computer work, reading, classroom work etc. They are not for outdoors, TV or for constant wear.
Golden Rule: If you can touch it with your hands you should have your training spectacles on to see it.
- Most need the training spectacles for 12-18 months we can reduce or eliminate the need to wear them anymore.
- We will do a 6 week review to ensure the training lenses are developing better accommodative stamina.
- If there is little or no change after this time, visual therapy will also be considered, however, this is only needed in about 33% of cases.
- Visual therapy requires 4-6 in practice visits along with home based activities being done in between visits.
Note:
These are generalised guidelines and each case may need to be evaluated on the individual basis. Treatment duration will depend on the particular patient’s condition.
CONVERGENCE INSUFFICIENCY
WHAT IS CONVERGENCE INSUFFICIENCY?
The textbook definition for Convergence Insufficiency is:
“A neuromuscular abnormality of the binocular system characterised by an inability to converge the two eyes or to sustain the two eyes converged.”
or more simply… this means that the individual has difficulty keeping both eyes turned in and pointing at the same thing when they are doing near work.
This is not eyesight or muscle problem but rather an adaption to the stress of keeping the two eyes turned in (converged) for long periods. The brain chooses to let one eye drift out and suppresses the image from the that eye (so no double vision) and hence alleviates stress of keeping both eyes turned in.
TESTING FOR CONVERGENCE INSUFFICIENCY
The diagnosis of with Convergence insufficiency is based on 4 main clinical criteria:
1. When the eyes drift out (Exophoria) more at near than in the distance.
- 4 prism Dioptres.
2. Receded Near Point of Convergence.
- Can’t turn both eye in to fixate something inside 6 cm form their nose.
3. Reduced ranges of maintain single clear near vision.
- Called near Base out Fusional Ranges.
- 15 prism base out cause loss of fusion.
CAUSES
The reason for the development of a Convergence problem are not fully understood. There are two theories that have been suggested but not scientifically proven as yet:
- Poor convergence development:
Due to genetics or poor natural development and with the commencement of school and having to do more prolonged near work (like learning to read) this problem then becomes apparent.
- The volume of prolonged near work has out stripped the stamina to cope with it. This can also happen in the adult eye, especially if you are doing a lot of stressful near centred task (eg new job involving more close work, study, prolonged computer work, fine sewing etc).
SYMPTOMS
The symptoms associated with Convergence insufficiency are usually related to the task that produces the stress, i.e. prolonged near centred tasks. The symptoms may include, but are not limited to the following:
- Visual Stress Symptoms.
(Red eyes, sore eyes, transient blurry vision and/or headaches.
- Difficulty sustaining near visual attention. (may actually avoid near task).
- Abnormal posture adaptations such as pulling books closer.
- Occasionally double vision or the letters moving or running.
TREATMENT
Double blind studies done in 2008 showed that:
- Visual Therapy intervention was the most successful treatment (72%).
- Doing Pencil Push Ups was successful in 43% of cases.
- Computer Convergence Training was successful in 33% of cases.
We use the following treatment strategy:
1. Training Spectacle lenses for all close work.
- These are a little like braces on crooked teeth that gradually straighten the teeth and are then are removed.
- The training lenses help alleviate or reduce the visual point stress and allow the individual to develop better convergence stamina.
- The more they are worn for near work the sooner better convergence abilities are developed, the sooner the spectacles are no longer needed.
2. Eye Exercises. (Visual Therapy)
- Visual Therapy on its own is slow to improve stamina problems for the simple reason that for every half hour of therapy might be done at night time; the child/adult has usually been doing 5 or 6 hours of “Anti-therapy” during the day (i.e. demanding close work causing near point stress and the eyes drift apart.)
DURATION OF TREATMENT
Generally the training lenses are needed to be worn for all close work including computer work, reading, classroom work etc. They are not for outdoors, TV or for constant wear.
The Golden Rule: If you can touch it with your hands you should have your training spectacles on to see it.
- Most need the training spectacles for 12 – 18 months before we can reduce or eliminate the need to wear them anymore.
- We will do a 6 week review to ensure the training lenses are developing better convergence abilities.
- If there is little or no change after this time Visual Therapy will also be considered.
- This is only needed in about 40% of cases.
- Visual Therapy requires between 4 to 6 in-office visits (2-3 weeks apart) along with home based activities been done between visits.
- NB: These are generalised guidelines and each case may need to be evaluated on the individual basis. Treatment duration will depend on the particular patient’s condition.
CONVERGENCE EXCESS
WHAT IS CONVERGENCE EXCESS?
The textbook definition for Convergence Excess is:
“A sensorimotor anomaly of the binocular vision system, characterized by a tendency for the eyes to over converge at near.”
In plain English, this means that the individual has difficulty keeping both eyes pointing at the same thing when they are doing near work without the eyes drifting in.
WHAT CAUSES A CONVERGENCE PROBLEM?
The two main reasons for developing a Convergence problem are:
1. Poor convergence development:
- Due to genetics or poor natural development.
- With the commencement of school and having to do more prolonged near work (like learning to read) this problem then becomes apparent.
2. The volume of prolonged near work has out stripped the stamina to cope with it.
- This can also happen in the adult eye, especially if you are doing a lot of stressful near centred task (eg new job involving more close work, study, prolonged computer work, fine sewing etc).
SYMPTOMS
The signs and symptoms associated with convergence excess are often related to prolonged, visually-demanding, near centred tasks such as reading. They may include, but are not limited to, the following:
- Visual Stress Symptoms (red eyes, sore eyes, transient blurry vision and/or headaches).
- Difficulty sustaining near visual attention (may actually avoid near task).
- Abnormal posture adaptations such as pulling books closer.
- Occasionally double vision or the letters moving or running.
TREATMENT
Convergence excess is often successfully managed by prescription of therapeutic lenses and/or prisms. However, optometric vision therapy may also be required.
1. Training (therapeutic) spectacle lenses for all close work.
- These are a little like braces on crooked teeth, they gradually straighten the teeth then are removed.
- The training lenses help alleviate or reduce the visual point stress and allow the individual to develop better convergence stamina.
- The more they are worn for near work the sooner better convergence abilities are developed, the sooner the spectacles are no longer needed.
2. Eye Exercises. (Visual Therapy)
- Visual Therapy on its own is slow to improve stamina problems for the simple reason that for every half hour of therapy might be done at night time; the child/adult has usually been doing 5 or 6 hours of “Anti-therapy” during the day (i.e. demanding close work causing near point stress and the eyes drift in.)
DURATION OF TREATMENT
Generally the training lenses are needed to be worn for all close work including computer work, reading, classroom work etc. They are not for outdoors, TV or for constant wear.
The Golden Rule: If you can touch it with your hands you should have your training spectacles on to see it.
- Most need the training spectacles for 12 – 18 mths before we can reduce or eliminate the need to wear them anymore.
- We will do a 6 week review to ensure the training lenses are developing better convergence abilities.
- If there is little or no change after this time Visual Therapy will also be considered.
- This is only needed in about 33% of cases.
- Visual Therapy requires between 4 to 10 in-office visits (2-3 weeks apart) along with home based activities being done between visits.
- NB: These are generalised guidelines and each case may need to be evaluated on the individual basis. Treatment duration will depend on the particular patient’s condition.
WHAT IS MYOPIA?
Myopia (short-sightedness) is one of the most investigated areas within vision science. Yet we still do not fully understand why myopia develops and how to stop it.
POSSIBLE CAUSES
- For myopia to occur the eyeball has to grow longer (change in axial length).
- In the past this axial length change was considered to be due to genetics, as myopia tends to run in families.
- The rapid increase of myopia over the last 50 years seems to coincide with the increase in literacy and industrialisation in most countries.
- This could indicate that high near visual demands and visual stress may also be a causal factor in developing myopia in some individuals.
- The general conclusion is that myopia is due to a combination of genetic and environmental factors.
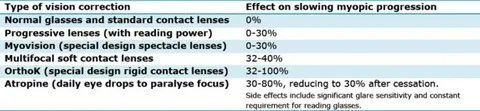
MYOPIA CONTROL
Myopia control is the area of science dedicated to slowing down or stopping the progression, or worsening of myopia in children and young adults. The following table is a compilation of over 30 research papers on myopia control, published up to and including 2013:
View This Animation
MANAGEMENT ALTERNATIVES
Based on all the accepted research we recommend the following treatment options as most likely to stop or slow the progression of myopia:
1. GOOD VISUAL HYGIENE:
- Good visual habits will reduce any near visual stress that may or may not be contributing to the development or progression of myopia. Either way, reducing near visual stress is a good thing for any visual system.
- Good visual hygiene includes not getting too close to near work (not inside your knuckle to elbow distance).
- Take regular breaks by looking away from your near work every 5 mins. If you notice a blur when you first look away it is time to take a longer break.
- Avoid prolonged close work while tired or sick as this may also increase near point stress and stimulate more myopic development.
2. MORE OUTDOOR ACTIVITY:
- A child with two myopic parents is at a six times greater risk of becoming myopic than a child with no myopic parents. A child with one myopic parent is at three times greater risk. This can be true even if you (the parent) didn’t become myopic as a child. Myopia can also occur without any family history at all.
- A recent Australian study found that students who combined high levels of near work with low levels of outdoor activity were more likely to become myopic, whereas students who combined low levels of near work with high levels of outdoor activity were more likely to stay longsighted.
- This was confirmed by a Singapore study which also found that lower amounts of outdoor activity increased the odds of becoming myopic.
3. SPECTACLE LENSES OR CONTACT LENSES TO REDUCE PERIPHERAL HYPEROPIC BLUR:
- In a myopic person, the central retina is myopic, but the peripheral retina is actually hyperopic, or long sighted. It is thought that this stimulates the eyeball to grow causing the myopia to increase.
- Some new spectacle and contact lens designs aim to reverse detrimental peripheral optics so that the peripheral focus is on, or in front of, the retina – similar to a non-myopic child.
4. SPECTACLE LENSES TO REDUCE NEAR VISUAL STRESS:
- Wearing plus lenses (or less minus) for close work has the effect of reducing the focusing (accommodative) demand and makes it easier to keep the eyes turned in (converged).This will reduce near visual stress.
- Studies have found this can be an effective way of slowing / reducing the rate of myopic progression.
5. ORTHO-K:
- The OrthoK technique uses special hard contact lenses which change the curvature of the cornea to neutralise the myopic prescription.
- These lenses are worn all night and removed each morning.
- Latest clinical and scientific research shows that OrthoK can slow the progression (worsening) of short-sightedness, or myopia, in childhood by around 50%. In some children OrthoK can even halt the progression of myopia.
6. ATROPINE TREATMENT:
- Atropine is an eye drop used to dilate the pupil and temporarily relax the eyes’ focusing mechanism. It has long been acknowledged that atropine also reduces the progression of myopia.
- Recently it has been shown that low-concentration atropine gives the benefit of slowing the myopic progression without the visual side-effects.
If you require any further information on any of these treatment options please do not hesitate to ask your optometrist.
VISUAL HYGIENE
WHAT IS VISUAL HYGIENE?
Good visual habits can reduce eye stress and reduce the likelihood of adverse visual adaptations. Please read the following hygiene points carefully.
- Take regular breaks during study and other sustained close work. Using a bookmark may help you get into the habit of doing this. Place the bookmark three of four pages in front of where you are reading. When you get to it, it will remind you to look up at something in the distance. Make sure it is clear, relaxing and closing your eyes for a few seconds. Look back down to your work and move the bookmark another three or four pages in front.
- Make sure you do not get too close to your work. You should not be any closer than the distance between your knuckle to elbow when placed against your nose. Again use the bookmark to remind you to check this periodically. You may be aware if the fact that you are pulling the work closer to you as you tire.
- Good lighting for all near work is important. For maximum efficiency, use general lighting in the room so you can see distance objects easily when you look up. Two desk lamps placed on either side of your work will eliminate shadows. Be sure the quality of your lights is adequate for comfort, but not too bright. Do not read after the lights have turned out or with a torch.
- Good posture ensures that you are at that knuckle to elbow distance from your near work. Avoid reading in bed or on the floor. Sit up to read.
- Tilt your book and work surface whenever possible to achieve its presentation parallel to your face. Once all school desks were sloped to ensure this. A sloped top desk is a valuable aid to good visual function since it presents the task in a desirable position and also helps to support the bode in a balanced posture. Try to obtain a desk and chair suitable to the child’s size.
- Do not sit any closer to the TV than five times the screen width or two of the child’s body lengths. Young children naturally sit very close to the TV because they want to involve all of their senses. Gently encourage them to sit further away. Use adequate room lighting. It is important to note that vision develops better with active tasks such as sports and reading, so children should be encouraged to limit passive TV viewing times.
- Off-set high demand tasks with outdoor games requiring adequate distance viewing, such as golf, tennis and bike riding. Do not let your child constantly read.
- Restrict close work and reading during acute illness. At such times our personal energy reserves are lower and our ability to sustain the visual stamina required will be reduced. High fevers appear to put the visual system at risk of significant change.
- Avoid reading and other sustained near activity while travelling by car. At such times, movements greatly add to your eye focus, eye pointing and teaming demands.
- When writing, a pencil grip using the thumb and the two next fingers enables best manipulation. The grip must allow visual inspection of the paper during performance. The writing material should be aligned according to handedness on the slope to desk at correct work distance.
LEARNING RELATED VISUAL PROBLEMS
WHAT IS LASER AUTO REFRACTION?
We have gathered some different ways to on how to help your child become better at reading. These different ideas have been gathered from a number of sources, as well as written by ex-teacher Francis Hansen. These ideas are not meant to replace any reading techniques by their teacher or at school.
Pick one or two activities and prepare one for morning and night.
As your child achieves in the activity go onto another. The child MUST always be achieving. If it is too hard, find an easier activity. Do not let him/her get bored with it. Keep it light, short and varied.
Some children (and parents!) are too tired at night to do extra. Make the effort to get up 10-15 minutes earlier in the morning to do these activities when you and your child are fresh.
Make a reading or activity time everyday for everyone in the house when the television is NOT allowed to be turned on. This will prevent the child rushing through the task and being preoccupied with what the other family members are watching on TV.
It has been shown in a number of studies that if Dad works with the child, progress is achieved faster, especially if the child is a boy. This, of course, is not always practical but we found that by sharing the activities as parents with one working at night and the other in the morning, we achieved the best results with our children.
As parents we can get very frustrated, tired and even angry with our child because they are not learning, didn’t listen or will not concentrate. At these times it is important to remember that our child does not choose to learn, listen or concentrate. Consider how frustrated, tired and angry your child must feel inside because he/she cannot live up to your expectations.
Of all the people in your child’s life you are the one who must be patient, loving and understanding of them and their problems. The chances are that their peers and siblings may not.
HELPING YOUR CHILD LEARN TO READ
“Children who are not spoken to by live and responsive adults will not learn to speak properly. Children who are not answered will stop asking questions. They will become incurious. Children who are not read to will have few reasons for wanting to learn to read”. “The Read – Aloud Handbook” by Jim Trelease.
TALKING AND LISTENING
The words that we use for talking, we use for reading. Talk to your child and have your child talk to you. In this way you will increase your child’s vocabulary which will help make him/her interested in many different books and also show that he/she understands what he/she reads.
- Have your child talk about what they see, hear, smell and feel. By describing what we see, we pay more careful visual attention and improve visual discrimination skills. Play eye spy etc.
- Have your child tell about past experiences, today’s experiences, and what you plan to be doing in the future. Have him describe what it will be like at different events, eg a picnic on the weekend, etc this will help the child develop better time concepts.
- Dictate stories that your child tells you. This will show your child that reading is talking “written down”.
- Children enjoy making nonsense words particularly when they get the idea and become competent at it.
- The Alphabet Game: Beginning with “A” each player must think of an object beginning with “A” in turn. It’s good to do this to a rhythm e.g. clap knees three times and the player must take his/her turn on the fourth hand clap or miss out a go.
- When reading together, and words like “the” or “one” cannot be sounded out. Say to the child: “There are some funny words that you just cannot sound, and you have to remember them and this is one. Look at it and remember it”. You may then have the child write it out on his chalkboard or make up a card to put in his/her bedroom so that he/she can look at this often.
PROMOTING THE DESIRE TO READ
“Richer than I could never be, I had a mother who read to me”
None of us like doing things we don’t do well. If your child isn’t a particularly good reader or doesn’t enjoy it the reading is a boring laborious chore. This is particularly true if we have to sound out and stumble through each word as we read. You can help develop sight word recognition and word attack but predominantly that will be the teacher’s task. As a parent often the best thing we can do is to keep the child motivated and interested in reading.
Here are some suggestions we have found helpful.
- Read aloud to your child. We find time for what we value. Regular reading aloud strengthens your child’s reading, writing and speaking skills. Let him/her choose the book and you do the reading. As you go point out details and information about the pictures that go with the story and ask your child questions about what’s happening. These special read aloud times will build relationships between you and your child. Those ten minutes spent reading aloud may be the only time you spend with that particular child all day. Do that everyday and your child will be yours forever.
- Read yourself. If you read your child will realize that you value reading and he /she will realize that reading is important.
- Use a tape recorder. As you read your child’s favourite stories, put them on to tape so that he/she can have a story to listen to and to help him/her read their favourite books anytime that he/she wants. Your library has many of such tapes available freely for you to borrow.
- A rating and progress chart. Each time you read a story to your child have him or her rate how they feel about the book. In this way the child will see that you are reading lots of books together and that some books are better than others. Try and set a goal to read “X” number of books per week or per month. Make it realistic according to the ability of your child and how enthusiastic he or she is.
- Children love to receive letters in the post for themselves. Why not go to your local bookstore and enquire if they have a “Kids Club” he/she could join to receive a magazine for them to read. There is a “Kids Club” with Puffin Books on the web. See www.penguin.com.au.
- Try and build your own library by buying a book each week if you can afford it. A greatly underutilised resource is our own public library. It does not cost anything to join, only the time to go the library and select a book.
LEARNING HOW TO READ
“Six Sausages Sitting on a Snake”
Language forms the basis of reading. Symbols are used to represent sounds so that words become sounds written down. This is not true for all words especially in the English language. When the child goes to school, he/she is “taught to read”. This means the child is taught to:
- Break words up into sounds (phonic decoding).
- Recognise written words as having a spoken meaning (sight words).
As parents we can appreciate the importance of developing good language skills before we expect our child to develop good reading skills. Here are some suggestions to help these abilities.
WAYS TO IMPROVE PHONIC DECODING
- Discuss sounds and play listening games. These games develop confidence in the child to read and write simple stories and words. Always have the child watch your lips as you say the words.
- Have the child talk about Mum and Dad’s activities. His/Her skill in visualisation will determine the number of objects and activities he/she can classify and he/she will be building the associations between visualisations, articulation and language in this procedure.
- Show your child an interesting picture. Let him/her hold and handle it first. Encourage him/her to talk about the picture and his/her visual inspection of it. Help him to increase the length of his/her sentences, which describe the picture.
- Encourage your child to imitate the sounds of an aeroplane, train, car, clock, animals etc. The ability to imitate these sounds gives him/her control of the lips, tongue and throat positions for good speech.
- Have your child give the opposite to words you say, such as black when you say white; little when you say big etc.
- Give your child oral directions involving two activities, then three, four and more as he/she can accomplish them. For example: pick up the magazine, put it on the table and sit on the chair. Repeat until your child can do it just as you have said. If difficulty is encountered, repeat each direction as he does it until he/she can do them following the instruction.
This activity develops auditory span and when the child has learned to hear it completely and comprehensively the first time it is stated, it can save the parents and teachers much time and repetition. Thus, as he/she grows and learns to depend on his/her auditory discriminations, his/her judgements and decisions will be sped up. Always make him/her stop and watch your lips as you give instructions. Again this will help reinforce visual-auditory integration.
WAYS TO IMPROVE WORDS THAT SHOULD BE RECOGNISED BY SIGHT
- Label objects in the house: wall, chair, television etc. It might look strange to some one visiting your house but you will be surprised how quickly it helps your child recognise the words by sight. Sometimes take them down and play matching games.
- Cut out pictures of every day things, e.g. tree, bird, car, dog and write down separate labels in lower case letters. Have the child then try and match the word with the picture.
- Make up word-cards with different activities on them and have the child do what the word says, e.g. run, hop, work, play, etc.
- Make up word-cards for adverbs e.g. walk quickly, slowly, sadly, noisily, quietly, happily, etc.
- Make up word-cards for prepositions. Have him/her put an object in, on, under, beside, below, above, behind a box etc.
- Make up word-cards for adjectives. Have him bring you something blue, red, big, little, striped, smooth, hard, soft, fuzzy, etc.
Neurological Impress Method: A multi-sensory method to help your child become a better reader.
SEE & PERCEIVE
HEAR & LISTEN
SAY & UNDERSTAND
OBJECTIVES
- To promote fluency of reading
- To train the eye to move freely across the page
- To develop rhythm and flow of oral reading
- To increase confidence and enjoyment of reading
Time taken:
Ten minutes per night for eight weeks.
Material: Reading material slightly below the child’s present reading level.
METHOD
- Child sits next to and in front of the parent so that the parent’s voice (HEARING) is close to the child’s ear.
- Together, they read out loud (SIGHT and SPEECH) from the same book with the child’s finger tracing across the page beneath the words as they are reading.
- The finger MUST coincide with the words read as the child’s eye follows the finger, and must look directly at each word as it is HEARD and SPOKEN.
NOTES
- Do not correct the words the child doesn’t know.
- Do not question the child about the text.
- Read so that the child can keep up with you.
- Tell the child to use the same inflexion, phrasing and emphasis that the parent does.
- Avoid material that is too difficult.
- Do not be tempted to read longer than 10 minutes.
- If the child does not respond after four weeks then the method is perhaps unsuitable for the child. At 8 weeks, significant improvement should be noticed.
HELP PROMOTE WRITING SKILLS
“That Starting Point of Curiosity About the Written Language is an Interest in Scribbling and Drawing.”
Before your child learnt to walk he had to learn to crawl. The crawling motor skills had to be developed before the finer and more difficult walking skills. The same is true for writing. Before your child can learn the fine eye-hand manipulative skills involved in writing he/she must have mastered the gross body, neck and eye-hand skills that form the fundamental basis to those finer writing skills.
Here are some suggested activities to help this.
- Chalkboard Activities: Let your child scribble with chalk in both hands and encourage him/her to cross the midline. You can draw little scribble patterns at the top of the chalkboard and try and get the child to copy them. Butchers paper can be used. Other activities such as finger painting, playdough and lego are also good.
- Give your child lots of practice on a chalkboard drawing nonsense shapes before attempting to do them on paper, symbols such as letters and numbers. If your child doesn’t have the ability to draw a square, triangle, cross, circle or diamond then he is not ready to learn the more complex shapes of letters and numbers.
- Always have paper and pencil available for the child. The starting point of curiosity about written language is an interest in scribbling and drawing. From this develops an interest in copying objects, and letters of the alphabet. Display his/her paperwork in the home.
- Write stories the child dictates.
- Write Stories together.
- Parents write the beginning or end of a story and have the child write the other part.
- Parents write a chapter of a story and the child continues the next chapter. See how far the chapter takes you before you complete the book.
- Write letters to friends and relatives.
- Write messages for other members of the family rather than speaking the message.
HELP YOUR CHILD BECOME A BETTER SPELLER
As a child’s writing develops, they constantly look for new words and for new ideas many of which they don’t know how to spell. As the ideas flow into writing, to stop and research the spelling words from dictionaries and other sources will impede the flow of those ideas. Far better initially to guess the spelling of the word and fill in the correct spelling later rather than spoil the flow of writing. You might like to speak to your child’s teacher as to how it works.
Here are some things we have found useful to help your child become a better speller.
- The Look and Write Method. Look at the word and say it to yourself. Cover it over, close your eyes and see it. Write down the word; check whether it is spelt correctly. If not repeat the method again.
- Multi-sensory approach. Research has shown that the more senses involved in learning to spell the better their attention. Hence if a child has to see, say and do something in regards to learning, the word he /she will learn it faster.
- Ball Method. Write each spelling word on a separate piece of paper in large, black, small case letters. Hold up one card at a time saying the word to the child. Have the child repeat the word back to you. Have the child then spell the word out while he is bouncing a tennis ball or larger ball if required. The child bounces the ball on bounce each letter e.g. “CAT” is Cat (bounce); C (bounce); A (bounce); T (bounce); CAT (bounce). Sometimes vary this method by having the child clap out the word, stamp it out, trampoline, skipping rope or balance board.
This method takes the tension out of the “spelling homework” and the child relaxes and the learning takes place almost as if the action of the ball stamps the words into the child’s visual memory.
- Encourage your child to write at home, as spelling is used constantly. Try to provide a place where writing can be done. “Exhibit” his/her writing. Encourage the child to use a dictionary.
- Work through other ways such as with scrabble words and magnetic letters. There are several commercial spelling games on the market but these are only good once the child has become a fairly competent speller, e.g. Junior Scrabble, Boggle etc.
- It’s hard to spell a word you do not know the meaning of. Research shows that children read and spell words they “own”, i.e. boat, mother, sister, dog, etc. Concrete words like these he/she owns and understands. He/She knows the meaning, as they are real to him/her. He/She can imagine the meaning. Abstract words which are difficult for the child to understand, e.g. behind, on, under, special; need thorough discussion about the meaning so that the child can understand the word and therefore own it. He/She has to be able to imagine the meaning of the word.
- Spell words on recording device or computer.
GET IN TOUCH
Contact Us
Thank you for contacting us.
We will get back to you as soon as possible.
We will get back to you as soon as possible.
Oops, there was an error sending your message.
Please try again later.
Please try again later.
© Copyright 2020 | All Rights Reserved |
Western Optical Hansens Optometrist
| Web Design by
ACM Digital